Editor: Yassine came all the way from Belgium to attend our San Diego event in August 2017 and submitted this story about his daughter to us afterwards about how they are using a Low Carb Diet For Type 1 Diabetes. We felt we had to share it with you.
 On August 19th 2016, our 11-year-old daughter was diagnosed with type 1 diabetes. The care team at the hospital did a phenomenal job at nursing her back to health and training us in the main aspects of diabetes management, namely diet and insulin regimen.
On August 19th 2016, our 11-year-old daughter was diagnosed with type 1 diabetes. The care team at the hospital did a phenomenal job at nursing her back to health and training us in the main aspects of diabetes management, namely diet and insulin regimen.
One week later we were back home and implementing the diet we were taught, structured around specific amounts of carbs for each meal and snack and corresponding insulin doses. We were using 4 daily injections of a fast-acting insulin (NovoRapid, similar to NovoLog, typically 22 units per day) and slow acting insulin (Lantus, typically 11 units at bed time).
During our training at the hospital the educators were very clear that the long-term complications of diabetes (retinopathy, nephropathy, micro and macro-vascular disease, etc.) were due to high blood sugars (>160mg/dL, aka “hyperglycemia”, or “hypers”) inflicting progressive damage to specific cells over years of poor glycemic control.
Low blood sugars (<60mg/dL, aka “hypoglycemia” or “hypos”), in comparison, can create significant discomfort (dizziness, sweating, trembling, etc.) but our care team explained that they were not dangerous per se (unless a severe hypo happens while the diabetic is driving for example).
We were also taught that the key health metric used to track glycemic control was glycated hemoglobin (aka “HbA1c”). It is a good estimation of the average blood sugar levels over approximately the last 3 months. Healthy non-diabetic people typically have A1c values between 4.5 and 5.5%. diabetics are typically higher than 6.5%. Most diabetes care official guidelines try to keep patients’ HbA1c levels below 7.5% for kids and 7% for adults.
All the complications of diabetes are associated with high A1c level. According to the studies on diabetic cohorts, higher risks of serious complications appear for A1c higher than 5.5%
(data from DCCT (1996) (1), Stratton et al. (2000) (2), Khaw et al. (2004) (3), Feinman et al. (2015) (4)).
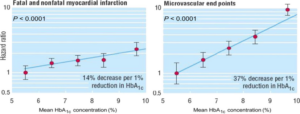
Dependence of risk for myocardial infarction and microvascular end points on hemoglobin A1c. Data adjusted for age at diagnosis of diabetes, sex, ethnic group, smoking, presence of albuminuria, systolic blood pressure, high- and low-density lipoprotein cholesterol, and triglycerides. UKPDS
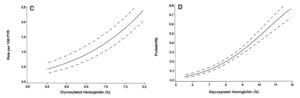
The absolute risk of sustained retinopathy progression (hazard rate per 100 patient-years) in the combined treatment groups as a function of the updated mean HbA1c during follow-up in the DCCT estimated from a Poisson regression model with 95% confidence band. C: rate vs. values of HbA1C 58%. D: cumulative incidence (probability) over 9 years of treatment vs. HbA1c
This was very surprising to us. If the odds of extremely serious complications started from A1c levels higher than 5.5%, why would the objective be to be at 7%? Why not shoot for normal blood sugar levels for diabetics?
The answer we were given was that it was very hard to control blood sugars in general, and that it was not realistic to aim for normal blood sugars and A1c levels, so if we were below 7%, we were already “reducing” the risk for long term complications. The curves above represent instantaneous (C) or 9-year cumulative risk levels (D). My daughter will hopefully live way beyond 9 more years, and over her full expected lifetime, the cumulative risk corresponding to a 7% A1C is dramatically higher than that of an A1C of 5.5%. Conclusion: @ 7% A1C, we are definitely NOT reducing the risk for long term complications to an acceptable level, only normal A1C levels (as in healthy non-diabetic subjects) would do.
We thought that we should investigate ways that we can improve glycemic control and test the hypothesis from our diabetes care team that it is “impossible to have normal blood sugars” in our daughter’s case.
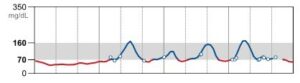
We are lucky to be able to use a continuous blood glucose monitor (Abbot’s Freestyle Libre), which provides us with a continuous curve of blood glucose measurements throughout the day (technically, the sensor captures sugar concentration in the skin interstitial tissue and extrapolates blood sugar, but in our case, the estimate we get from that are very close to a 20-minute time-shifted curve of actual blood glucose as measured by a standard finger-prick glucometer method). Here is how a day of our daughter’s blood glucose levels looked like on the recommended diet and insulin regimen (on a good day…).
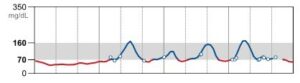
After each meal (containing typically 30-70g of carbs), blood glucose would go up, then the insulin we had injected 5 to 15 minutes before the meal would kick in and bring it back down. These significant variations are due to the recommended high carb diet. We were taught to count the carbs and inject a corresponding dose of fast-acting insulin.
We found it extremely hard to reduce or remove the variations in the curve above. We experimented by slightly changing the insulin doses, the timing of the injections with respect to meal times, etc. But we learnt that the speed at which carbs impact blood sugar depends on many things (what you eat with the carbs, in what order, etc.). The absorption speed of injected insulin is also variable. Bottom line, we found that, in perfect agreement with what we were told at the hospital, we could not maintain a low variation of the blood sugar curve, at least with the recommended diet.
So, to recap, in order to avoid long term diabetic complications, we want to maintain low A1c levels. To do so, we need to maintain low average blood sugars. Since the curve varies significantly due to high carb meals, low average blood sugars mean very frequent hypos. Although we understand hypos are not serious issues per se, they have a significant impact on our daughter’s daily life, including relatively severe discomfort multiple times a day that affect her classroom focus and overall morale.
In other words, as long as the blood sugar curves have such levels of variance, we have to choose between the 2 undesirable outcomes of higher either A1c (long term risks) or many hypos (short term issue).
We therefore started thinking about how we could lower the variance of the glycaemia curve. Given that dietary carbs have by far the highest impact on blood sugar levels, we started considering lower carb diets and, accordingly, lower fast-acting insulin doses.
When we lowered the number of carbs per day from 160-200g per day to 35-40g a day, the results were spectacular (right hand curve is for low carb).
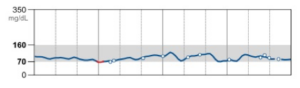
Switching to a low carb diet was a very effective way to normalize our daughter’s blood sugars.
Using large doses of carbs and insulin makes any tiny variation in absorption rates or timing result in a hyper or a hypo. Using lower doses of carbs and insulin mean the unavoidable variations in timings and absorption rates result in tiny peaks or valleys instead. Smaller inputs lead to smaller errors from unavoidable mistakes. As the peaks and variance become much smaller, it becomes possible to have a normal average blood sugar levels without the crippling hypos she used to undergo. She has been on this diet for a couple of months now, her blood sugars typically vary between 60 and 130mg/dL in the day with averages between 80 and 90, her A1c 3 months after diagnosis was 5.2%, the hypos went from more than 10 to less than 3 per week and the hypers went from 2 per week to 0. This outcome is actually consistent with the rare academic studies we have been able to dig up on the use of lower carb diets for type 1 diabetics (Nielsen et al. (2005) (5)). We were by the way surprised to find so few studies on this topic. The sample sizes are quite low and the long term impacts poorly known as few studies go beyond a couple of years.
We wondered how our daughter would take to a low carb diet. I guess we are lucky that she does not have a sweet tooth. We compiled a list of recipes from websites like dietdoctor.com or ditchthecarbs.com. We created weekly meal and snack plans from these recipes. Then we tested them and asked our daughter for rate each recipe. To this day we keep testing new recipes and replacing the ones she does not approve of. Giving her control of the meal plan is our way of making her part of it and making sure we are not subjecting her to meals she does not like. She says she is reassured by her blood sugar curves and likes her meals so far. We do no hesitate to make exceptions (e.g. birthday parties, when she asks for sushi, etc.), we just give her the corresponding dose of fast-acting insulin. We are also experimenting with many low carb sweetened recipes so she does not feel deprived of cakes, sweets and deserts. The online resources for this are abundant and the recipes fairly easy to follow.
This low carb approach to stabilize blood sugars is still an exception among diabetics. Very few doctors recommend this diet for multiple reasons, most of which are still unclear to us. The 27 co-authors of Feinman et al. (2015) are strongly advocating for the use of low carb diets for diabetics, claiming that the available evidence for the upsides is compelling enough while that of the alleged risks is not. Davis & Runyan’s book (6),and Dr. Bernstein’s (7) Diabetes Solution are 2 very useful sources on this topic.
At the same time, most doctors, including our original endocrinologist, do not recommend low carb diets. They mention many long-term risks (growth, liver metabolism, oxidative stress, microvascular issues, etc.). The problem is, we have found many research papers tying all these problems to high blood sugars, not low carb diets. The pattern we have seen is that most situations where we see these problems also involve high A1c levels, which normal blood sugars specifically help avoiding.
The bottom line is: we are in charge of our daughter’s health, and to the best of our knowledge a low carb diet tackles the biggest long term risk for her health. We are perfectly happy changing our mind and diet if
- She does not like it
- The demonstrated downsides of low cab diets are more problematic than the increased risk of diabetic complications associated with A1c levels higher than 5%
For now, the former is not true and we have not been able to find compelling evidence for the latter.
The Facebook group Type1grit was a tremendous help during this whole process. It is a extremely active and helpful community of type 1 diabetics and their parents following the low carb diet described in Dr. Bernstein’s diabetes solution book. The members are very supportive and combine a wide variety of expertise areas and experience levels. I have still to ask a question in that group’s page that was not followed within hours, sometimes minutes, by a useful and supportive reply. This community is wonderful and an invaluable help in the emotional rollercoaster following the diagnosis.
Now let’s take a look at some of the common warnings we got from different doctors or dietitians about low carb diets:
1. You mean you eat more Fats?
Reducing carbs means increasing at least one of the other two macronutrients. We follow the protein guidelines for her age and weight (and appetite). The main change in her diet is a significant increase in the quantity and variety of vegetables, as well as a significant increase in protein (about 2g/kg/day, she weighs about 40kg) and natural fats (1.5g/kg/day – by “natural” we mean no prepared industrial dishes, trans-fats, etc., but the fats naturally present in meats, fish, dairy products, etc.). We have naturally looked into the recent literature on dietary fat, focusing on RCTs and systematic meta- analyses, and our conclusion is that dietary fat (especially saturated fat) is not convincingly associated with heart disease (see Harcombe et al. (2016) (8), Santos et al. (2012) (9), Kuipers et al. (2011) (10), among others). We are aware this is complex and extensively researched, that different types of fats play different roles, that long term studies tend to be observational cohort ones while RCTs testing for causality tend to be relatively short term (less than 2 years). That being said, we have found no compelling evidence to discourage us from using a low carb diet to stabilize blood sugars. Gary Taubes’ book, Good Calories, Bad Calories (2007), proposes an in depth literature review on this topic and helped us tremendously in navigating this research field.
2. It may work, but it is not sustainable!
It is working for us for now, and our daughter loves the recipes. We understand that this might change dramatically as she grows up, hits teen age rebellious years, etc., but in the meantime we will have gained as many years as we can with normal blood sugars and we will have trained ourselves and her to makes delicious low carb meals. We allow exceptions (friend’s birthday cakes for example) and our daughter is in full control of the meal plan.
3. It is not possible to control blood sugars!
We are aware that blood sugar can be influenced by a myriad of factors (diet, exercise, weather, hormones, puberty, infection, etc.). We have already observed wild variations during an infection (a cold) and expect significant ones during puberty etc. We understand there are many factors we do not control, we just want to fix the one we do control.
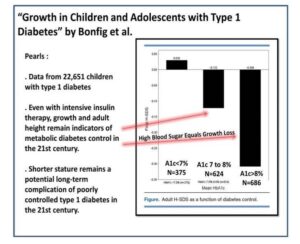
4. It will interfere with her growth!
This was a surprise to us, as we could not find out why sufficient protein, sufficient energy (from fat) and a wide variety of healthy vegetables would impair growth. We have found a few articles (Bonfig et al. (2012) (11)) about growth curves for type 1 diabetics and they show an association between high A1c and stunted growth. Our low carb diet allows us precisely to keep A1c low, so we are still looking for evidence. We are checking regularly her height and weight. 5 months from diagnosis, she is still tracking nicely with her pre-diabetes growth curves (75th percentile for height and 50th for weight), time will tell us if she is drifting away from them.
We are still looking for all the evidence we can find to help us understand the risks we may be increasing, but so far we have found nothing compelling to lead us to change what we are doing.
Both my wife and I are engineers and profound believers in science. We usually follow to the letter the doctor’s recommendations. In this specific case, we are for now convinced that the nutrition research does not support the alleged evils of a properly formulated low carb diet. We are actively in search of evidence either way and are fully ready to change our approach in the face of compelling evidence. We are not certain of our approach, especially in the face of so much push back from most doctors, but in our honest opinion the available evidence is not consistent with this pushback, and the alternative would be to submit our daughter to higher A1c levels, and there is ample compelling evidence that that is not a favorable outcome.
[Make sure you get to one the LowCarbUSA® events and see people who are changing lives and meet others whose loves have been changed forever!]
References
- Control, T. D., Trial, C., & Control, T. D. (1996). The absence of a glycemic threshold for the development of long-term complications: The perspective of the Diabetes Control and Complications Trial. Diabetes, 45(10), 1289–1298. https://doi.org/10.2337/diabetes.45.10.1289
- Stratton, I. M., Adler, A. I., Neil, A. W., Matthews, D. R., Manley, S. E., Cull, C. A., … Holman, R. R. (n.d.). Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational
- Khaw, K.-T., Wareham, N., Bingham, S., Luben, R., Welch, A., & Day, N. (2004). Association of Hemoglobin A 1c with Cardiovascular Disease and Mortality in Adults: The European Prospective Investigation into Cancer in Norfolk . Annals Of Internal Medicine, (141), 413– 420.
- Feinman, R. D., Pogozelski, W. K., Astrup, A., Bernstein, R. K., Fine, E. J., Westman, E. C., … Worm, N. (2015). Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition, 31(1), 1–13. https://doi.org/10.1016/j.nut.2014.06.011
- Nielsen, V., Jönsson, E., & Ivarsson, A. (2005). A Low Carbohydrate Diet in Type 1 Diabetes: Clinical Experience – A Brief Report. Upsala J Med Sci, 110(3), 267–273.
- The Ketogenic Diet for Type 1 Diabetes, Ellen Davis, M.S. and Keith Runyan, M.D. (2015)
- Bernstein RK. Dr. Bernstein’s diabetes solution: the complete guide to achieving normal blood sugars. 4th ed. New York: Little, Brown and Co; 2011
- Harcombe, Z., Baker, J. S., DiNicolantonio, J. J., Grace, F., & Davies, B. (2016). Evidence from randomised controlled trials does not support current dietary fat guidelines: a systematic review and meta-analysis. Open Heart, 3(2), e000409. https://doi.org/10.1136/openhrt- 2016-000409
- Santos, F. L., Esteves, S. S., da Costa Pereira, A., Yancy, W. S., & Nunes, J. P. L. (2012). Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obesity Reviews, 13(11), 1048–1066. https://doi.org/10.1111/j.1467-789X.2012.01021.x
- Kuipers, R. S., de Graaf, D. J., Luxwolda, M. F., Muskiet, M. H. A., Dijck-Brouwer, D. A. J., & Muskiet, F. A. J. (2011). Saturated fat, carbohydrates and cardiovascular Netherlands Journal of Medicine. https://doi.org/10.3945/ajcn.2008.26285
- Bonfig, , Kapellen, T., Dost, A., Fritsch, M., Rohrer, T., Wolf, J., & Holl, R. W. (2012). Growth in children and adolescen ts with type 1 diabetes. The Journal of Pediatrics, 160(6), 900–3.e2. https://doi.org/10.1016/j.jpeds.2011.12.007
- Flotats Bastardas, M., Miserachs Barba, M., Ricart Cumeras, A., Clemente Leon, M., Gussinyer Canadell, M., Yeste Fernandez, D., … Carrascosa Lezcano, A. (2007). Hepatomegalia por deposito de glucogeno hepatico y diabetes mellitus tipo 1. Hepatomegaly due to Glycogen Storage Disease and Type 1 Diabetes Mellitus, 67(2), 157–160. https://doi.org/http://dx.doi.org/10.1016/S1695-4033(07)70577-5
- Jain, S. K., McVie, R., & Bocchini, J. A. (2006). Hyperketonemia (ketosis), oxidative stress and type 1 diabetes. Pathophysiology. https://doi.org/10.1016/j.pathophys.2006.05.005
- Roh, H.-T., Rhyu, H.-S., & Cho, S.-Y. (2014). The effects of ketogenic diet on oxidative stress and antioxidative capacity markers of Taekwondo athletes. Journal of Exercise Rehabilitation, 10(6), 362–366. https://doi.org/10.12965/jer.140178